Case being discussed here :
23 year old, man, paraplegic with Potts spine
Link for the case being discussed below:
Q. Jaw jerk-
1+ normal or abnormal, normal grading of jaw jerk. Where is the lesion if jaw
jerk is exaggerated . Afferent or
efferent? Motor supply got muscles of mastication. Nucleus of Jaw jerk
location?
A. In a positive response, sudden stretching
of the masseter muscle causes reflex contraction, moving the jaw briskly
upward. With the patient’s jaw slightly open, the clinician can elicit the
reflex by tapping with a reflex hammer directly on the chin or on a tongue
blade resting on the lower teeth or tongue.
The afferent impulse for this reflex is formed by
the sensory portion of CN V and efferent by motor portion of CN V.
An exaggerated jaw jerk, sometimes appearing
with clonus , implies bilateral disease above the level of the pons (e.g.,
pseudobulbar palsy).In patients with spastic tetraparesis, for example, an
exaggerated jaw jerk excludes cervical cord disease and points to pyramidal
tract disease above the pons.
Most of the
motor supply for muscles of mastication is by the mandibular branch of
trigeminal nerve.
Q. Paraparesis
- spinal cord level?
|
https://www.spinalinjury101.org/details/levels-of-injury
High cord
lesions C1-C4:
Quadriplegia
+ may have difficulty to breath + may have difficulty to control bowel and
bladder + speech maybe impaired
Low Cervical
Nerves C5-C8:
Corresponds
to arms and hands + may be able to breath or speak
https://www.spinalinjury101.org/details/levels-of-injury
Thoracic Nerves:
T1-T5:
Affects
muscles of upper chest + midback and abdominal muscles + paraplegia
T6-T12
Paraplegia +
muscles of trunk and abdomen + little / no voluntary bowel/ bladder movements
https://www.spinalinjury101.org/details/levels-of-injury
Lumbar
Nerves L1-L5
Reduced
power in both the lower limbs ( walks with braces or wheelchair) + little or no
voluntary bowel or bladder
Sacral
Nerves S1-S5:
Affects hips
and legs – most likely will be able to walk + little or no voluntary bowel and
bladder
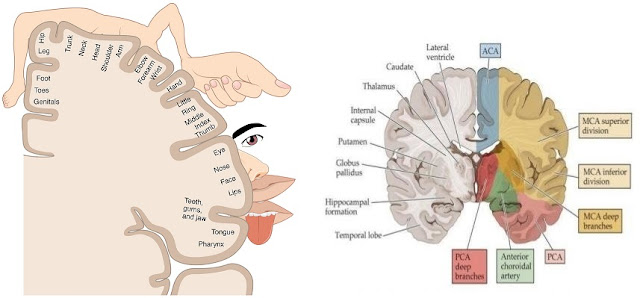
Q. Cortical
causes of paraplegia:
A. Cerebral
Diplegia,
Superior sagittal sinus thrombosis,
Parasagittal meningioma,
Thrombosis
of unpaired ACA,
Gunshot injury of this area,
Internal hydrocephalus
Q. Vascular
area affected in cortical region to cause paraplegia, Motor Homunculus:
A. ACA
territory

https://www.spinalinjury101.org/details/levels-of-injury
ACA Territory supplies the basal and medial aspects of the cerebral hemispheres & extends to the anterior 2/3rd of the parietal lobe.
When the ACA Territory is affected - Contralateral Paraparesis + hypoesthesia of lower limbs + Altered mentation, judgement, insight + Apraxia + Gait clumsiness + Bowel & bladder involvement
Presence of primitive grasp + suck reflexes
https://www.spinalinjury101.org/details/levels-of-injury
MCA – putamen, anterior limb of internal capsule, lentiform nucleus, external capsule. The main branch of MCA supply lateral surface of cerebral cortex to the posterolateral occipital lobe.
When MCA territory is affected - C/L Facial & arm motor and sensory is affected
Homonymous Hemianopia + gaze towards the affected side
If non dominant side is affected - Hemineglect is seen

PCA – Brainstem, Cerebellum, thalamus, auditory & vestibular centers of the ear, medial temporal lobe, visual occipital cortex.
Homonymous Hemianopia - visual disturbances + memory loss + alexia
Q. Difference of Bulbar and pseudobulbar palsy & causes
| BULBAR PALSY | PSEUDO BULBAR PALSY | |
| SITE OF LESION | Nuclear + Infranuclear | Supra nuclear |
| WEAKNESS | Flaccid | Spastic |
| ATROPHY | ++ | - |
| FASCICULATIONS | ++ | - |
| DYSPHAGIA | Severe, Nasal Regurgitation | Coughing more than nasal regurgitation |
| SPEECH | Nasal | Heavy, Spastic Donald Duck speech |
| FACIAL WEAKNESS | LMN Type | UMN Type |
| GAG REFLEX, JAW JERK, FRONTAL RELEASE SIGNS, EMOTIONAL INCONTINENCE | - - | ++ + |
| CAUSES | MND, GBS, Syringobulbia, Poliomyelitis, Subacute Meningitis, Neurosyphilis | MND, Multiple Sclerosis, High brainstem tumors, Head injury |
Link for further details of the case being discussed below
https://manisha420.blogspot.com/2020/06/june-6th2020-medicine-intern-log-hello.html?m=1
Q. 57 yr, F, with paraplegia with areflexia in lower limbs , dorsal and spinothalamic tract involvement what could be your clinical diagnosis?
There could be complete spinal cord injury secondary to extradural or intradural lesions.
Areflexia could be due to spinal shock.
Q. Myelopathy causes

Q. MRI FINDINGS:
Spinal cord compression can be seen at T4 and L2 level secondary to Metastasis
Q. What is Kyphosis, Scoliosis, Lordosis ?
Kyphosis is exaggerated outward curvature of the thoracic region of the spine resulting in a rounded upper back.
Scoliosis is abnormal lateral curvature of the spine.
Lordosis is inward curvature of spine
A gibbus deformity is a short-segment structural thoracolumbar kyphosis resulting in sharp angulation.
Could be congenital & Acquired
Congenital could be due to Achondroplasia, Mucopolysaccharidosis, Cretinism
Acquired could result from Pott's disease, osteoporosis, Vertebral metastasis
Link to the case being described
https://pri422.blogspot.com/2020/06/medicine-intern-log.html?m=1
18 year old, man, GBS
Q. Causes of high stepping gait
Also known as Neuropathic gait, Steppage gait.
Is a gait abnormality characterized by foot drop due to dorsiflexion. So the foot touches the ground first which makes the patient raise his foot higher off the ground than normal while walking.
Causes: Usually seen in Peripheral Neuropathy
Can be caused by Syphilis, AML, CMT, Poliomyelitis, Spinal disc herniation
Q.Where do you see a Drunken Gait?
Drunken gait is seen in cerebellar strokes
Q. Causes of peripheral neuropathy and drugs causing peripheral neuropathy
Q. Evaluation of peripheral neuropathy based on the history
Images from Harrison Principles of Internal Medicine
Image from Harrison Principles of Internal Medicine
Q. Types of gait and how do you localize the lesion based on the gait
Here's a link to different types of gait and localization of the lesion
https://geekymedics.com/gait-abnormalities/
Q. What is the most important feature of UMNL ? - Spasticity + Hyper reflexia
Q. When is a Lumbar Puncture performed in AIDP ? In the second week from the onset of symptoms.
Elevated CSF protein - 1-10g/L without accompanying pleocytosis ( <50 cells/uL). Transient rise in leucocytes is seen by the end of first week from the onset of symptoms. Persistent raise of leucocytes would suggest to rule out other causes of viral etiology, neurosarcoidosis, HIV, lymphoma or leukaemia causing infiltration of the nerves.
Q. Treatment of AIDP
Treatment should be started as soon as a diagnosis has been made.
IVIG - as 5 daily doses of a total dose of 2g/kg body weight or
A course of plasmapharesis of 40-50ml/kg 4-5 times in 7-10 days.
Q. What happens to patients who do not receive treatment for AIDP?
Link to the case being discussed below:
18 yr, man with B/L LL weakness
Q. Cremastric reflex importance
When the medial aspect of the thigh is stroked, this stimulates the ilioinguinal nerve sensory fibers which activates the motor fibers of genitofemoral nerve causing the cremaster muscle to contract and elevate testis.
It is absent in testicular torsion, UMNL,LMNL, spine injury L1-L2.
Q. Demyelinating diseases symptoms :
Ocular Manifestations:
Blurred vision, U/L vision loss, Oscillopsia, Diplopia
Motor Symptoms:
Spasticity, Hyperreflexia, balance difficulties
Sensory Symptoms:
Paresthesia, Dysestheisia, Proprioceptive deficits, MS Hug, L'hermitte's sign
Autonomic Manifestations: Bowel & bladder dysfunction
Link to the case being discussed below :
35 yr old woman with a H/o of pulmonary TB 4 yrs back with right hemiplegia
Presence of any signs of meningeal irritation - Only presence of Neck rigidity due to meningeal irritation
Hemorrhage clinical features - Sudden onset of headache as described by the patient, Visual disturbance, multiple episodes of seizures, vomiting, syncope, Painful eye movements
RCT on aspirin and Clopidogrel in the management of ischaemic stroke
SPARCL - STROKE PREVENTION BY AGGRESSIVE REDUCTION IN CHOLESTEROL LEVELS
* This study was conducted among 4731 patients who had a stroke or TIA within one to six months before study entry, had low-density lipoprotein (LDL) cholesterol levels (100 to 190 mg/dl) , and had no known coronary heart disease
*This was a double-blind prospective study
2365 patients received 80 mg of atorvastatin per day whereas 2366 received placebo.
During a median follow-up of 4.9 yrs, 265 patients receiving atorvastatin and 311 patients receiving placebo had a fatal or nonfatal stroke. The atorvastatin group had 218 ischemic strokes and 55 hemorrhagic strokes, whereas the placebo group had 274 ischemic strokes and 33 hemorrhagic strokes.
In patients with recent stroke or TIA and without known coronary heart disease, 80 mg of atorvastatin per day reduced the overall incidence of strokes and of cardiovascular events, despite a small increase in the incidence of hemorrhagic stroke.
MATCH Trail on Aspirin + Clopidogrel vs Clopidogrel alone in Ischaemic Stroke
https://pubmed.ncbi.nlm.nih.gov/15276392/
7599 high-risk patients with recent ischaemic stroke or transient ischaemic attack and at least one additional vascular risk factor who were already receiving clopidogrel 75 mg/day.
A randomised, double-blind, placebo-controlled trial to compare aspirin (75 mg/day) with placebo.
Duration of treatment and follow-up was 18 months. The primary endpoint was a composite of ischaemic stroke, myocardial infarction, vascular death, or rehospitalisation for acute ischaemia
596 (15.7%) patients reached the primary endpoint in the group receiving aspirin and clopidogrel compared with 636 (16·7%) in the clopidogrel alone group. Life-threatening bleedings were higher in the group receiving aspirin and clopidogrel versus clopidogrel alone.Major bleedings were also increased in the group receiving aspirin and clopidogrel but no difference was recorded in mortality.
Adding aspirin to clopidogrel in high-risk patients with recent ischaemic stroke or transient ischaemic attack is associated with a non-significant difference in reducing major vascular events. However, the risk of life-threatening or major bleeding is increased by the addition of aspirin
TRIAL ON ASPIRIN VS PLACEBO
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2796.2003.01233.x
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2796.2003.01233.x
Patients with ischaemic stroke but not complete paresis were included. Totally, 441 patients (220 aspirin, 221 placebo) completed the trial.
The trial was randomized, double-blind and placebo-controlled.
Tablets Aspirin 325 mg or placebo, water solvable, were administered orally once a day for five consecutive days.
Neurological assessments were carried out three times daily during the treatment period to detect progression of at least two points in the Scandinavian Stroke Supervision Scale.
Patient outcome was followed up at discharge and at 3 months.Aspirin treatment did not significantly reduce the frequency of stroke progression. Amongst aspirin‐treated patients, stroke progression occurred in 15.9% as compared with 16.7% in the placebo group, which is less frequent than expected. The relative risk was 0.95 (95% CI 0.62–1.45) in the treatment group.
Patient outcome was followed up at discharge and at 3 months.Aspirin treatment did not significantly reduce the frequency of stroke progression. Amongst aspirin‐treated patients, stroke progression occurred in 15.9% as compared with 16.7% in the placebo group, which is less frequent than expected. The relative risk was 0.95 (95% CI 0.62–1.45) in the treatment group.
As regards patient outcome at discharge and after 3 months, aspirin treatment did not show any difference.
Q. How does physiotherapy help
Physiotherapy helps by preventing muscle contractures and improves function & mobility after a stroke by repetitive task training and relearning day to day activities.
Q. How does a brain recover in 2-3 weeks
The initial recovery following stroke is most likely due to decreased swelling of brain tissue, removal of toxins from the brain, and improvement in the circulation of blood in the brain. Cells damaged, but not beyond repair, will begin to heal and function more normally.
The brain may actually create new nerve cells through neurogenesis.
Q. Contraindications for thrombolysis
Q. Auscultation of eyeball - comment and causes
Riesman's sign or Snellen-Riesman's sign is a clinical sign characterized by bruit heard over the closed eye.The Snellen-Riesman's sign is due to the hyperdynamic circulation and increased cardiac output in thyroid eye disease and hyperthyroidism.
Usually present in other conditions like Stenosis or occlusion of ICA, Atherosclerosis of carotid vessels, AV malformations, Cerebral hemangiomas, Anemia, AS, Beri Beri, Giant cell arteritis and Churg Strauss vasculitis.
* Link to the case being discussed
Q. Why is the patient have a cerebellar ataxia if the infarct is in the midbrain ?
This occurs when there is peduncular and red nucleus involvement.
* Link to the case being discussed:
Q. Parasitic causes of meningitis?
https://www.id-agram.com/
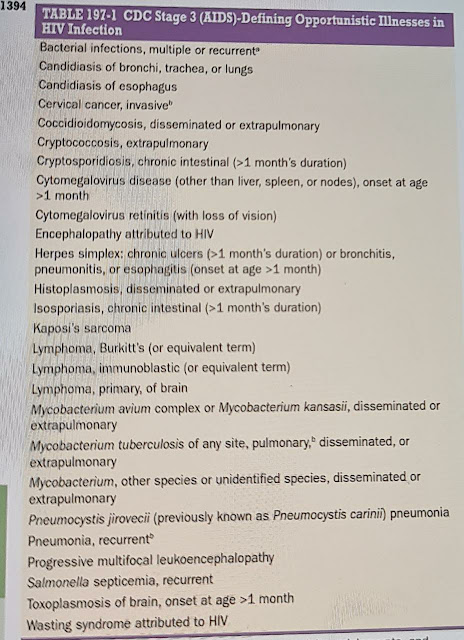
Q. Oppurtunistic infections in RVD
Images from Harrison Principles of Internal Medicine
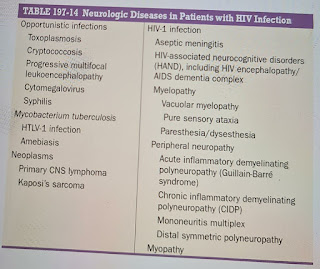
Q. Neurological manifestations in RVD
Q. Neurological manifestations in RVD
Image from Harrison Principles of Internal Medicine
Link to the case being discussed below
20 year old alcoholic man with weakness in both the lower limbs with areflexia, reduced vibrations
Points discussed :
* Use of thumb nail for the examination of plantar reflex
Q. Causes and Treatment in GBS - Already has been discussed
Q. Complications of GBS - ARDS, Pneumonia, Pressure sores, Septicemia
Q. When do you perform LP in GBS
* Presence of Hypopigmented patches - Leprosy needs to be ruled out
In GBS around 50 % patients have 7th & 12th cranial nerve involvement.
Q. QUECKENSTEDTS METHOD:
Test to determine whether or not the flow of cerebrospinal fluid is blocked in the spinal canal. The test is performed by putting bilateral pressure on the jugular veins during the course of a lumbar puncture. Normally there is a sharp rise increase in the pressure of the spinal fluid in the lumbar region within 10 to 12 seconds, and then a sharp fall when the pressure is released.
If there is no rise in the pressure of liquor cerebrospinalis, it is a sign of blocking of the subarachnoid channels.
Normally the CSF flow is 1 drop per minute which is considered to be normal pressure. Cough, sneeze, headache increases intra abdominal pressure and increases the csf flow rate.
Link to the case being discussed below :
18 yr old woman with paraplegia , areflexia
Q. Clinical examination of right sided pneumothorax
Trachea is pushed to the opposite side
Intercostal scar drained pneumothorax need to be looked for inspection
Asymmetrical chest expansion on the affected side
Hyper resonant note is heard on the affected side
Q. Type of Gait in Muscular Dystrophy - Waddling type of gait
Q. Difference between neuropathy, myopathy, myelopathy
Myopathy - Usually proximal weakness + pain + usually no sensory deficit + contractures maybe present + reflexes lost late
Neuropathy - Distal weakness + sensory symptoms + no contractures + relfex lost early
Myelopathy - UMNL/LMNL + Sensory deficit + bowel/bladder/sexual dysfunction
Q. Biochemical dysfunction causing this picture - Channelopathies / Phosphofructokinase deficiency
Q. Explain the following image
Middle aged, obese man, walking out of the restaurant, post dinner in a cold weather clenching his chest with a terror like expression, stepping upstairs with a briefcase falling off from his hand and a fallen cigarette on the ground - Image from Netters depicting Angina pectoris ( showing all the risk factors - age + obese + cold weather + smoker)
Link to the case being discussed below :
40yr woman with Quadriparesis
Q. Where could be the anatomical location ?
C4-c5 level
Q. Could the patient be in spinal shock? And stages of spinal shock ?